Alzheimer’s Research: Is This the Beginning of the End?
Recent discoveries in Alzheimer’s research provide hope for a cure.
A newly approved drug for Alzheimer’s disease that slows memory loss in this brain-damaging disorder holds promise, researchers say. But they caution against rushing to its use too soon.
“It’s exciting research—not a cure,” stresses Dr. Rosemary Laird, a geriatrician specializing in elder care and the principal investigator of ClinCloud Research (www.clincloudresearch.com), a clinical trial company in Viera, Fla. Because of potential side effects, she said, “it’s critical people consult a clinician who can help weigh the risks and benefits of this medication, prior to use.”
The FDA gave Leqembi (lecanemab) fast-track approval in early January, the latest of two therapies to target toxic changes inside the brain rather than ease symptoms caused by the disease’s relentless progression. Although widely viewed as a potential advance, at least in treating early disease, three deaths have been reported, and unanswered questions remain about the drug’s lasting benefit.
Where there’s an unmet medical need, as in Alzheimer’s, the federal agency reserves designation for quick treatment approval. Over 6 million Americans now face this incurable illness, which is expected to triple by 2060, according to the Centers for Disease Control and Prevention in Atlanta, Ga. Often described as the “long goodby,” Alzheimer’s begins with mild memory loss—often difficult-to-distinguish from normal aging—and with time, strips loved ones of their independence and all vestiges of self.
To slow disease progression, lecanemab removes damaging protein plaques that combine with a second protein inside the brain to begin tissue and nerve cell destruction. Early study results showed the anti-amyloid drug could delay disease progression by as much as 27 percent in those with mild memory impairment. That translated into a six-month slowdown in worsening symptoms—a brief reprieve from the anguish this illness exacts from patients and caregivers alike.
One caregiver, whose testimony appeared in the Congressional Record years ago, described the ordeal of taking her husband to the supermarket for groceries in the final throes of his illness. Because of severe mental confusion, he could no longer be left alone, she told legislators, so she wheeled him around in a cart while he chirped loudly like a parakeet and then soiled his pants.
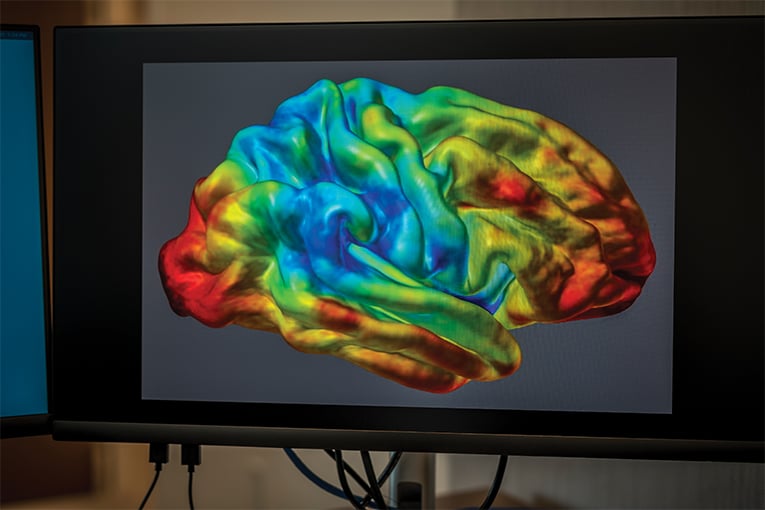
Similar distressing burdens remain the norm for many caregivers; today, the Alzheimer’s Association and other groups have stepped up efforts to help families cope. Though medical progress has been incremental, experts say they have unraveled the underlying pathways of this disease. Not only have scientists identified many risk factors, including genetic vulnerability to the disease, but they’ve also strengthened research ties to heart disease and overall fitness over the past few decades. And, through advances in imaging technologies, they’re able to visualize areas in the brain first compromised by disease.

Your brain is miraculous. It controls your movements, emotions and stores your memories. (ROBERTO GONZALEZ)
Researchers now know, for example, that the region of the brain most vulnerable to age-related deterioration and the earliest signs of Alzheimer’s lies in the hippocampus, which is located deep within the midbrain. The hippocampus helps regulate both memory and learning. It has emerged as the focus of much research because of its natural “plasticity,” according to Dr. Kirk Erickson, Director of Translational Neuroscience at Advent Health’s Neuroscience Institute in Orlando.
Although not the only area of the brain touched by Alzheimer’s as the disease progresses, Dr. Erickson said, plasticity means this region is “capable of being modified both for the worse and for the better.” He noted that the hippocampus is more likely to respond to treatments, such as aerobic exercise and other modifiable lifestyle factors, to stave off disease.
“There’s good research indicating that greater amounts of physical activity early in life can reduce an individual’s later risk of developing Alzheimer’s disease by about 50 percent,” Dr. Erickson said. Although how much exercise is needed to see benefits to brain health remains “one of the big questions in our field,” he said, most neurologists agree the minimum amount of exercise should follow public health guidelines: 30 minutes a day, five days a week. Whether more vigorous exercise will further reduce risk awaits further research.
Where experts seem to agree, however, is the link between risk factors for heart disease and those for developing Alzheimer’s disease. These include physical inactivity, high blood pressure, type 2 diabetes, obesity, and a smoking history. “So, keeping your heart happy will also work to keep your brain healthy,” Dr. Erickson said.
Clarifying other risks, such as genetic and heritable susceptibility, remains under intense study. Experts say a variant of a gene, known as APOE, plays a definite role in increasing risk, although it’s considered too early for routine gene testing. Many individuals who carry the variant never get the disease, complicating the genetic picture. A recent study found the highest concentrations of APOE-4, as it’s known, lie inside the hippocampus—an incremental boost to an understanding, perhaps, of a more aggressive disease.
None of the risks identified so far is more dominant than advancing age. They diagnose most cases in individuals over age 65 for reasons not fully understood. In Florida, where a growing number of elderly residents live, the state’s Department of Elder Affairs predicts some 720,000 people will be diagnosed with the disease by 2025—a 24 percent jump in cases in under five years.
Many in the field suggest such an alarming scenario may not be inevitable. Research has already shown, they say, that the damaging amyloid proteins accumulating in the brain start 10-to-15 years, or more, before the first signs of memory loss occur, providing an opportunity to intervene. That is considered especially promising at the front end of the disease, where some of the most significant progress has come.
“Failure to actively screen and monitor memory function earlier in life is not only unfortunate but also a missed opportunity to delay Alzheimer’s onset,” Dr. Erickson said. Many doctors are proactively working to change the disease’s screening status, he said, so that these tests take place annually, much as they do now for dental and primary care. Medicare does not provide coverage for cognitive assessments, currently under its annual wellness exams, until beneficiaries reach age 65.
Given a new understanding of mitigating or delaying risk, Dr. Laird said earlier screening, including baseline screenings, is sorely needed. Ideally, she said these tests should begin as early as age 50 in individuals with a family history who carry other defined risk factors.
Dr. Laird believes that individuals without these health concerns should consider screening for cognitive impairment or the loss of “episodic memory” between ages 55 and 60. If you lose this type of memory—usually the first to go—“you are not able to create a new memory of where you parked your car this morning or the dinner you had with a friend last month,” she said.
As with many other diseases, the value of early intervention seems self-evident. Not only can it enable those with Alzheimer’s to participate in clinical trials of promising innovative treatments as they become available, according to Dr. Laird, but it can also help family members and patients plan to manage the disease better.
She acknowledges that progress may feel too slow for those now desperately fighting the disease. “But, I believe, and I hope, we are in what I call the ‘germ theory era,’ where we are seeing true steps toward a cure.”